In February, we presented initial data of Labcorp's emerging humanized mouse platform utilizing human peripheral blood mononuclear cell (hPBMC) engraftment.
Our data using the NOD.Cg-Prkdcscid Il2rgtm1Wjl/SzJ (NSG) mouse resulted in identification of four hPBMC donors that exhibited a treatment window of at least 30 days post hPBMC injection, consistent T cell engraftment, and growth of two human xenograft models, MiaPaCa-2 (pancreatic) and A549 (NSCLC), that was robust in hPBMC-engrafted NSG mice.
We now present initial efficacy data demonstrating use of hPBMC-engrafted NSG mice bearing MiaPaCa-2 or A549 human xenografts following treatment with pembrolizumab (Keytruda®, anti-hPD-1).
Experimental Design
The objective of these studies was to evaluate the anti-tumor response of pembrolizumab against the MiaPaCa-2 or A549 human tumor models following the engraftment of hPBMCs in NSG mice. Animal care and use was performed in conformance with the Guide for the Care and Use of Laboratory Animals in an AAALAC-accredited facility.
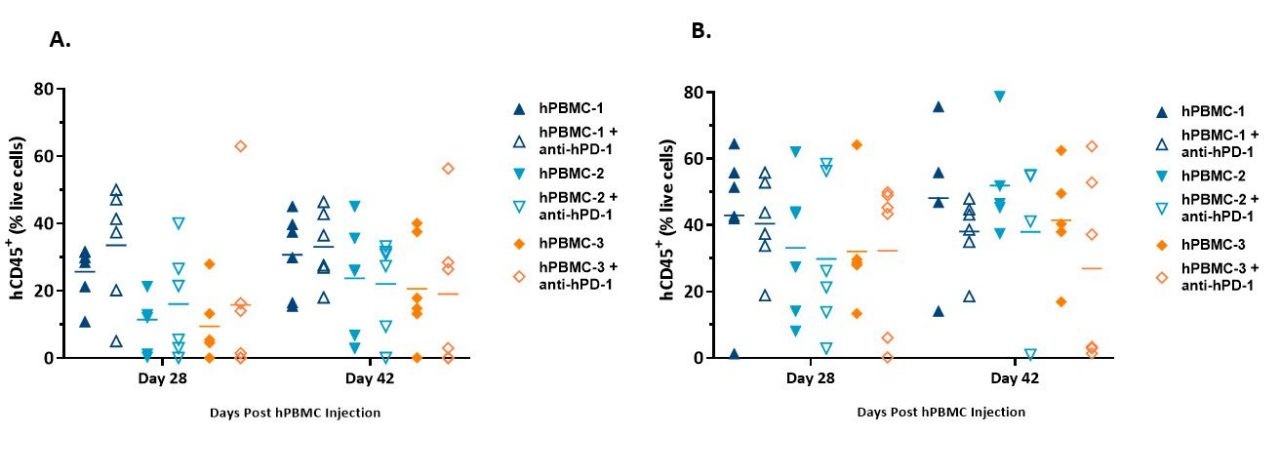
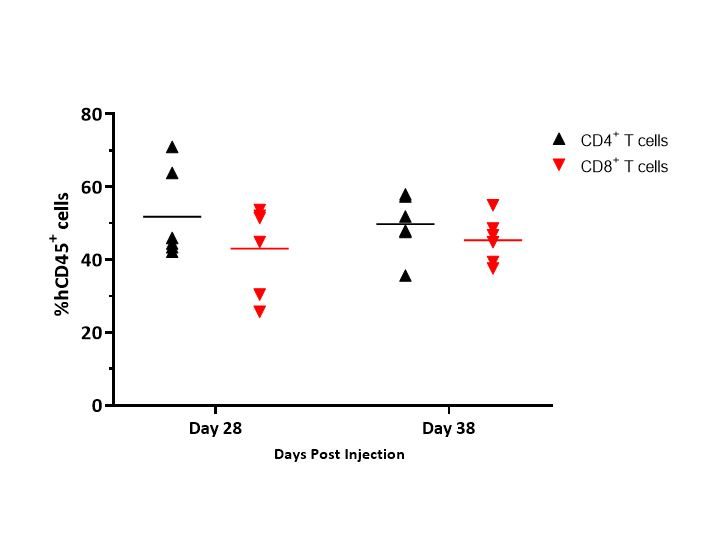
NSG mice (Jackson Laboratories, Bar Harbor Maine, USA, strain #0005557) were intravenously administered hPBMCs from three different normal healthy donors (Hemacare, Los Angeles CA, USA) once tumors became established (~105-118mm3). Treatment with pembrolizumab began the day after hPBMC injection. Response to pembrolizumab, evaluation of onset of Graft vs. Host Disease (GvHD)-like characteristics were determined, and whole blood was collected at two timepoints for flow cytometry analysis of human lymphocyte markers to confirm donor engraftment of CD45+ cells, including CD4+ and CD8+ T cells.
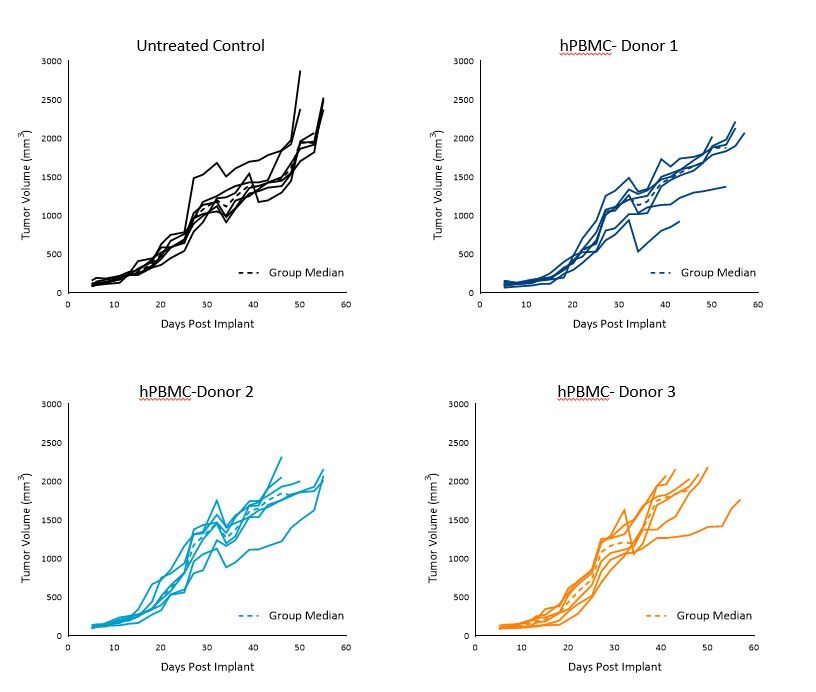
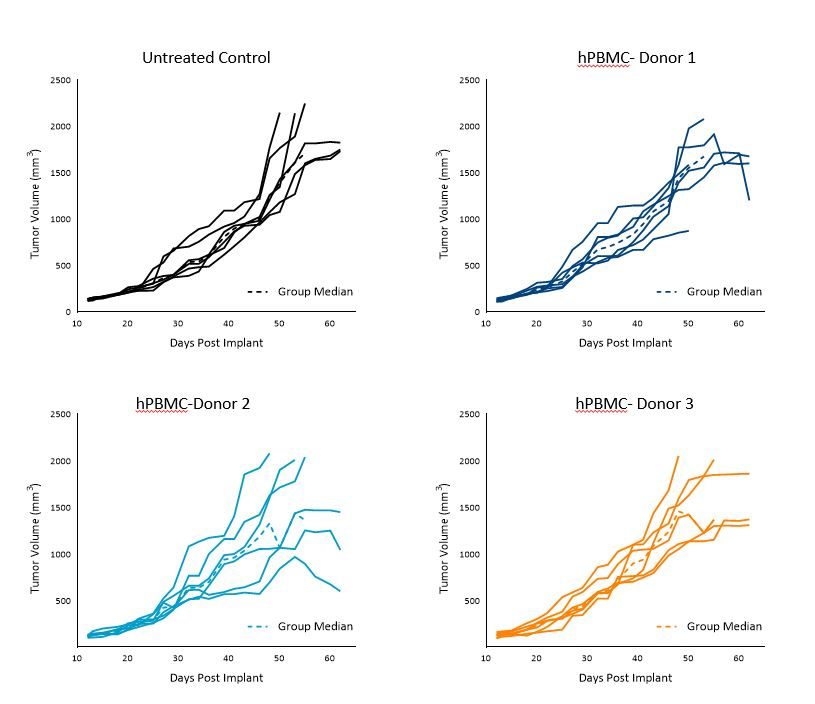
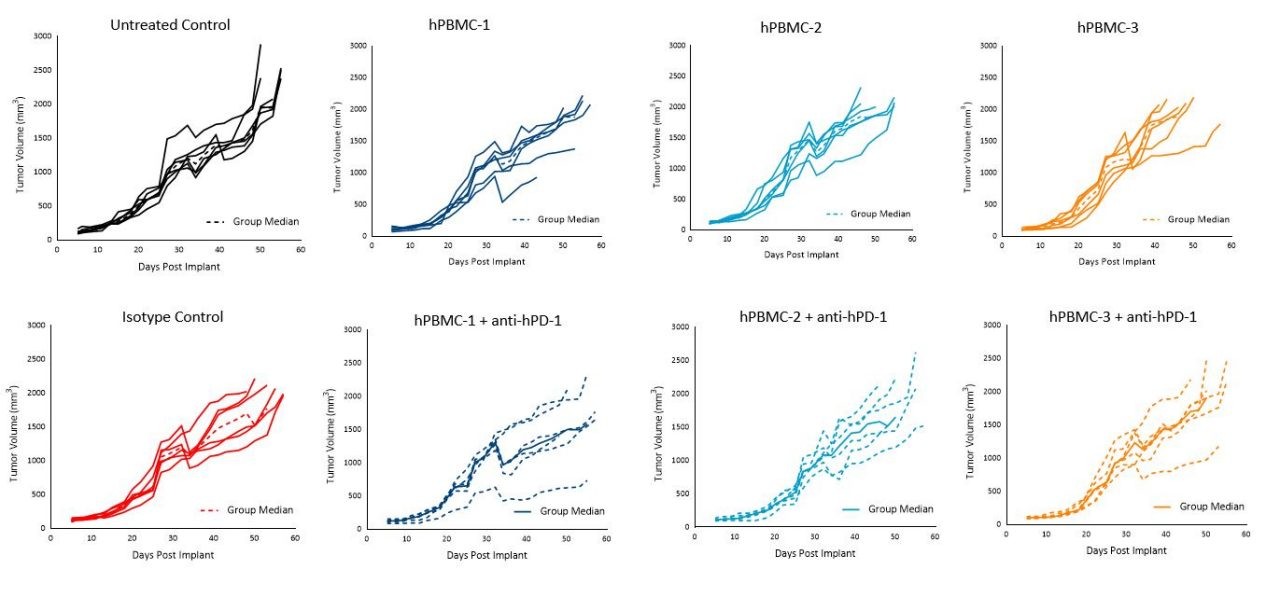
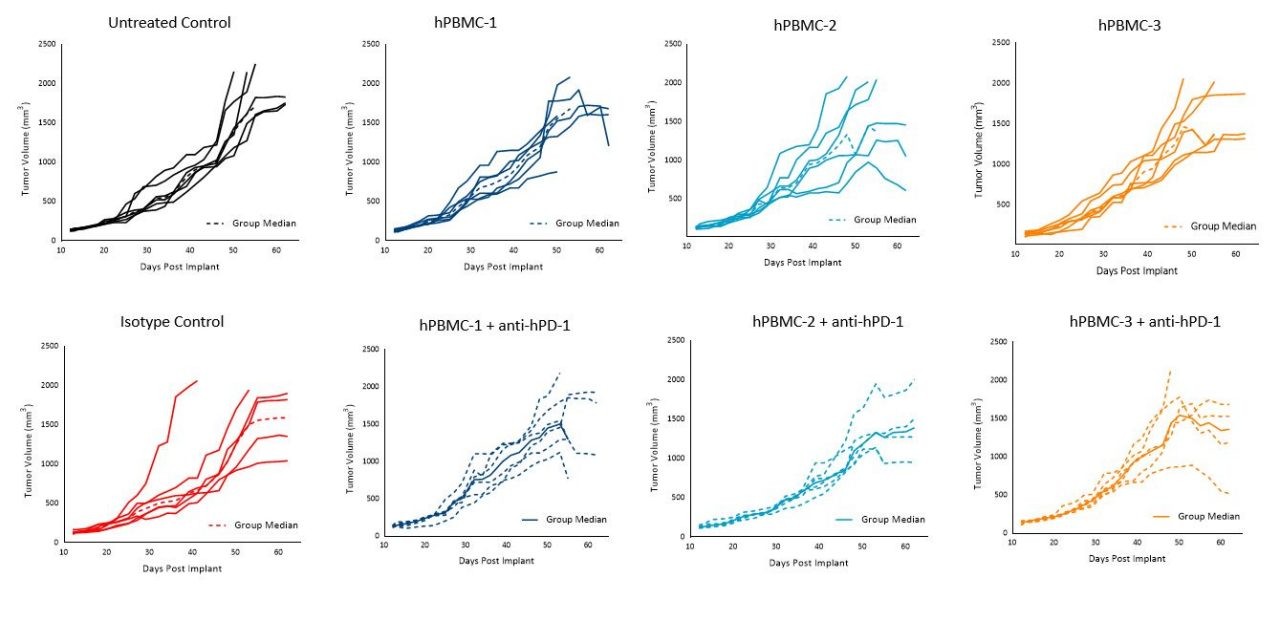
MiaPaCa-2 and A549 Control Tumor Growth in hPBMC Engrafted Mice
MiaPaCa-2 tumor doubling time (Td) in untreated control animals was ~7 days, Td in animals administered hPBMCs ranged from ~5 to 7 days across each donor group.
Tumors grew uniformly to a mean tumor volume of 1000-1200mm3 by day 36 across all three donors, however, some intragroup and intergroup variability was seen beyond day 36. Tumor growth before 1000mm3 did not appear to be impacted by engraftment of hPBMCs (Figure 1).
These results suggest that utilization of any of these three donors would be suitable for MiaPaCa-2 efficacy studies with a time to evaluation size (TES) of 1000mm3.